
Mid-Revenue Cycle Management/Clinical Documentation Improvement Market Size | CAGR of 7.3%
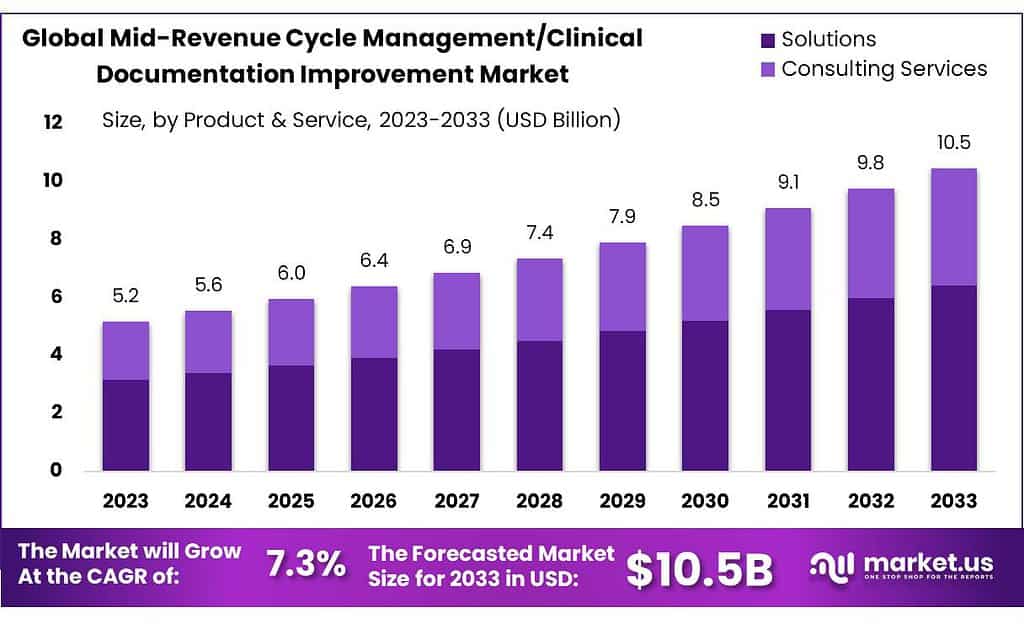
Mid-Revenue Cycle Management/Clinical Documentation Improvement Market size is expected to be worth around USD 10.5 billion by 2033, from USD 5.2 Bn in 2023, growing at a CAGR of 7.3% during the forecast period from 2023 to 2033.
The Mid-Revenue Cycle Management/Clinical Documentation Improvement Market refers to a segment within the healthcare industry focused on optimizing and streamlining processes related to clinical documentation and revenue cycle management. This market encompasses various software solutions, services, and technologies designed to enhance the accuracy, completeness, and efficiency of clinical documentation, particularly during the mid-revenue cycle phase.
The mid-revenue cycle encompasses activities that occur between patient care delivery and the billing process. It includes documentation tasks such as coding, documentation review, clinical documentation improvement (CDI), query management, and revenue integrity analysis. Effective management of this cycle is crucial for ensuring accurate coding, appropriate reimbursement, and compliance with regulatory requirements.
Key Takeaways
- Market Growth: The market is set to reach USD 10.5 billion by 2033, growing at a CAGR of 7.3% from USD 5.2 billion in 2023.
- Segment Dominance: Solutions hold a substantial 61.3% market share in 2023, offering features like clinical coding and charge capture to streamline processes.
- Healthcare Providers’ Share: Healthcare providers hold a dominant 35% market share in 2023, relying on solutions to optimize coding accuracy and enhance revenue capture.
- APAC’s Market Dominance: Asia-Pacific claims an impressive 61.5% revenue share in 2023, driven by rapid urbanization, construction activities, and a thriving automotive industry.
To understand how our report can make a difference to your business strategy, Inquire about a brochure at: https://market.us/report/mid-revenue-cycle-management-clinical-documentation-improvement-market/#requestSample
Factors affecting the growth of the Mid-Revenue Cycle Management/Clinical Documentation Improvement Market
- Regulatory Requirements: Stringent regulatory standards and compliance mandates drive the adoption of clinical documentation improvement solutions. Healthcare providers must ensure accurate and compliant documentation to meet regulatory requirements and avoid penalties, leading to increased demand for solutions that streamline documentation processes and ensure compliance.
- Shift towards Value-Based Care: The transition from fee-for-service to value-based care models emphasizes the importance of accurate clinical documentation in demonstrating quality of care, patient outcomes, and resource utilization. Healthcare organizations investing in clinical documentation improvement solutions aim to enhance documentation accuracy to support value-based reimbursement models and improve financial performance.
- Revenue Optimization: Healthcare providers seek to optimize revenue capture by improving documentation accuracy and completeness. Effective clinical documentation improvement initiatives lead to better code assignment, reduced claims denials, and increased reimbursement. As healthcare organizations strive to maximize revenue and financial performance, the demand for mid-revenue cycle management solutions continues to grow.
- Technological Advancements: Advancements in healthcare technology, such as electronic health record (EHR) systems, artificial intelligence (AI), and natural language processing (NLP), drive innovation in clinical documentation improvement solutions. Automated coding, CDI software, and predictive analytics tools enhance efficiency, accuracy, and productivity in clinical documentation processes, driving market growth.
Market Leading Segmentation
By Product and Service: Solutions: In 2023, Solutions held a dominant market position, capturing more than 61.3% share. This segment encompasses a wide range of software solutions designed to streamline and optimize mid-revenue cycle management and clinical documentation improvement processes.
By End-User: Healthcare Providers: In 2023, Healthcare Providers held a dominant market position, capturing more than 35% share. This segment includes hospitals, clinics, physician practices, and specialty care centers, relying on mid-revenue cycle management and clinical documentation improvement solutions to optimize revenue cycle processes.
By Product and Service
- Solutions
- Clinical Coding
- Clinical Documentation Improvements
- Charge Capture
- Clinical Documentation
- Diagnosis-related Grouping
- Pre-bill Review
- Consulting Services
By End-User
- Healthcare Providers
- Inpatient Settings
- Outpatient Settings
- Healthcare Payers
Key players
- Nuance Communications Inc.
- Chartwise Medical Systems Inc.
- Craneware
- 3M Company
- Streamline Health Solutions LLC
- Nthrive Inc.
- Dolbey Systems
- Optum Inc.
- Cerner Corporation
- Vitalware LLC.
Immediate Delivery Available | Buy This Premium Research Report@ https://market.us/purchase-report/?report_id=73406
Regional Analysis
In 2023, North America claimed the highest revenue share, surpassing 41.5%. The global Mid-Revenue Cycle Management/Clinical Documentation Improvement market saw significant shifts, with Asia-Pacific (APAC) emerging as a frontrunner, securing an impressive revenue share exceeding 61.5%.
Key Regions and Countries
- North America
- The US
- Canada
- Europe
- Germany
- France
- The UK
- Spain
- Italy
- Russia & CIS
- Rest of Europe
- APAC
- China
- Japan
- South Korea
- India
- ASEAN
- Rest of APAC
- Latin America
- Brazil
- Mexico
- Rest of Latin America
- Middle East & Africa
- GCC
- South Africa
- Rest of MEA
Drivers
One significant driver is the increasing focus on healthcare quality and regulatory compliance. With stringent regulations and guidelines governing healthcare documentation and coding, healthcare providers are under pressure to ensure accurate and comprehensive clinical documentation. CDI solutions help healthcare organizations enhance the quality and completeness of clinical documentation, leading to improved coding accuracy, better quality metrics, and enhanced compliance with regulatory requirements.
Moreover, the growing adoption of electronic health records (EHRs) and health information technology (IT) solutions is driving demand for mid-revenue cycle management and CDI solutions. EHR systems provide a platform for capturing and managing patient health information, facilitating documentation improvement processes, and streamlining coding workflows. Integration with CDI solutions enhances EHR functionality, enabling real-time clinical documentation review, coding validation, and compliance monitoring, thereby improving overall revenue cycle efficiency and accuracy.
Restraints
One big problem is how complicated and always changing the rules are for healthcare documentation and coding. Healthcare providers have to deal with lots of rules and standards, and they have to make sure their documentation and coding follow all of them. This can be tough for CDI solutions because they have to keep changing to keep up with the rules.
Also, CDI solutions cost a lot of money to set up and keep running. This can be a big issue for smaller healthcare places or doctor’s offices that don’t have a lot of money. They need to pay for software, hardware, training, and support, and it can add up fast. Sometimes, the cost is just too much for them, so they can’t use CDI solutions.
Opportunities
A big chance comes from the growing demand for better healthcare quality and following the rules. Healthcare places want to make sure patients get the best care and they meet all the rules. That’s where CDI solutions come in handy. These solutions can help make sure that all the paperwork and coding are accurate, making it easier for healthcare providers to meet quality standards and follow the rules.
CDI solutions that can quickly check documents, validate codes, and monitor rules are in a good spot to help healthcare providers meet their goals. Also, as more places use electronic health records (EHRs) and other tech tools, there’s a chance for CDI solutions to work together with these systems.
Challenges
One big challenge is the constant changes and complexity in healthcare rules and coding requirements. Healthcare providers have to keep up with a lot of rules and standards, and it’s tough to make sure all the documentation and coding are accurate and follow the rules. This makes it hard for CDI solutions to keep up because they have to keep changing to stay effective and follow all the rules.
Also, the cost of setting up and running CDI solutions is a major barrier for many healthcare places, especially smaller ones or doctor’s offices with limited money. CDI solutions need a lot of money upfront for things like software, hardware, training, and ongoing support. For some healthcare places, the cost is just too much, so they can’t use CDI solutions, which can lead to problems with accurate documentation and coding.
Conclusion
In conclusion, the Mid-Revenue Cycle Management/Clinical Documentation Improvement Market is characterized by significant growth driven by various factors. The dominance of Solutions underscores the importance of software solutions in streamlining revenue cycle management and clinical documentation improvement processes. Clinical Coding, Clinical Documentation Improvements (CDI), and Charge Capture also play vital roles in enhancing coding accuracy, revenue integrity, and workflow efficiency.
Get in Touch with Us:
Global Business Development Team – Market.us
Market.us (Powered By Prudour Pvt. Ltd.)
Address: 420 Lexington Avenue, Suite 300,
New York City, NY 10170, United States
Tel: +1 718 618 4351
Email: inquiry@market.us
Explore More Market.us Research Reports
Editor Details
-
Company:
- Wired Release
- Website:
